

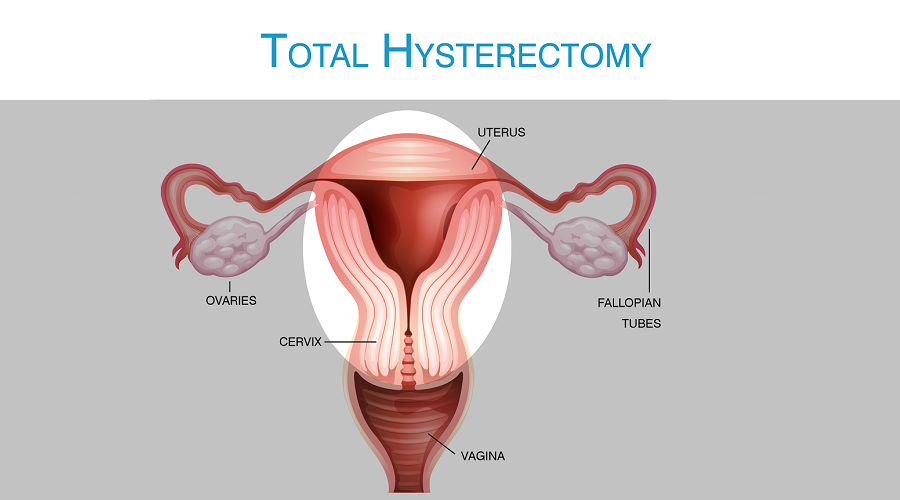
An abdominal hysterectomy is a surgical procedure that removes your uterus through an incision in your lower abdomen. Your uterus — or womb — is where a baby grows if you're pregnant. A partial hysterectomy removes just the uterus, leaving the cervix intact. A total hysterectomy removes the uterus and the cervix.
Sometimes a hysterectomy includes removal of one or both ovaries and fallopian tubes, a procedure called a total hysterectomy with salpingo-oophorectomy (sal-ping-go-o-of-uh-REK-tuh-me).
A hysterectomy can also be performed through an incision in the vagina (vaginal hysterectomy) or by a laparoscopic or robotic surgical approach — which uses long, thin instruments passed through small abdominal incisions.
An abdominal hysterectomy may be recommended over other types of hysterectomy if:
You may need a hysterectomy to treat:
A hysterectomy ends your ability to become pregnant. If you think you might want to become pregnant, ask your doctor about alternatives to this surgery. In the case of cancer, a hysterectomy might be the only option. But for other conditions — including fibroids, endometriosis and uterine prolapse — you may be able to try less invasive treatments first.
During hysterectomy surgery, your surgeon might also perform a related procedure that removes both of your ovaries and your fallopian tubes (bilateral salpingo-oophorectomy). You and your doctor should discuss ahead of time whether you need this procedure, which results in what's known as surgical menopause.
With surgical menopause, menopause symptoms often begin suddenly for women after having the procedure done. Depending on how much these symptoms affect your quality of life, you may need short-term treatment with hormones.
It is a minimal access surgical procedure which facilitates the removal of the non prolapsed uterus through vaginal route. Total Laparoscopic Hysterectomy (TLH) is an operation to remove the uterus with the aid of an operating telescope known as a laparoscope. This tiny instrument is inserted through a small cut in the abdominal wall and allows the surgeon to see inside patient's abdomen. The main benefit of this sort of hysterectomy is that patient will not need to possess a large cut in your abdomen as well as your recovery is generally much faster.
Cervix of the patient, or the neck from the womb, is also removed during this operation by laparoscopic technique. Uterine artery, Uterosacral ligament, cardinal ligament or Mackenrodt's ligament, all is dissected from above. Ovaries of the patient might be removed based on wishes of gynecologists as well as patients condition.
Not every patient is suitable for this total laparoscopic hysterectomy. If it's suitable for the patient, Gynaecologist will decide the type of hysterectomy require for the patient.
The operation will often take the time between one and two hours.
The patient will wake up with a tube inside bladder urinary catheter, an IV drip will be given to replace lost fluids, a drain tube, as well as an oxygen mask is required sometimes. Generally after 4 hours patient will be offered something to drink, and from next day the patient can start eating.
A patient will probably be able to eat breakfast the very next day. Additionally, a patient will be able to shower and also have the drip and catheter removed. Most patients are discharged on the second day.
All operations possess a small risk of complications. For many people, the risks are higher. For instance, there is chance of experiencing complications increases if patient smoke, have cardiovascular disease, diabetes or else patient are overweight.
Wound infection - all patient generally receive antibiotics within the drip to lessen the chance of infection.
Bleeding - half the normal women may require a blood transfusion during or following the procedure. Rarely, women will have bleeding following the operation will need to have another operation.
Blood clots in legs known as deep venous thrombosis – this is rare but sometimes thrombus will break off and travel to the lungs known as pulmonary embolism. Most of the patient are offered medication to reduce the danger of DVT.
As tissues heal inside the abdomen, loops of bowel or any other tissues may become stuck together known as adhesions, which occasionally is painful and may require further surgery to do adhesiolysis.
Severe complication such as a heart attack due to the strain on one's heart throughout the anaesthetic, as well as death is extremely rare.
Urine infection which may require antibiotics.
Damage towards the bladder or ureters.
Bowel damage is 1 in 1000 or major circulation system damage is one in 3000 for all laparoscopies, which may require a laparotomy in order to correct these complications. It is unusual, but occasionally this problem won't be recognised for some time.
If throughout the operation the surgeon decides that it is not safe to continue using the laparoscope it may be chose to convert to a regular abdominal open hysterectomy.
If patient have her ovaries removed and she was not already menopausal, patient may start to experience hot flushes.
A hysterectomy is irreversible so there is no chance of pregnancy following this operation.
Some pain as usual. a patient may even experience a period-like, cramping sensation in the abdomen or pain in the shoulders. This is the pain in the shoulder is thought to be due to the Co2 gas used to inflate the abdomen, which irritates the diaphragm. This, along with a sensation of bloating, usually lasts one or two days but in some cases, it will last few weeks. In case of pain patient should try simple analgesics such as paracetamol, Panadeine or Naprogesic. Severe pain is unusual. It is quite normal to possess a sore throat and some nausea after the operation. A sore throat is due to the endotracheal tube used whilst you are anesthetized. Analgesics and small quantities of fluids can help. Nausea and drowsiness are due to the anaesthetic itself.
A patient should leave dressings intact unless they are soiled or wet because the dressings are sterile. After a week patient may remove the dressing, and may leave the wounds open, or preferably cover with a Band-Aid. It is been shown that keeping wounds slightly warm and moist enhances healing. A patient should not apply antiseptic creams, Dettol, Betadine, methylated spirit etc towards the wounds without asking the gynecologists. These are unnecessary and in most cases bad for healing tissue. The easiest method to achieve a good scar would be to leave the wounds alone until healed. Sutures will need to be removed around five days in the date of operation.
Some redness of the wound is usual, especially around the site of the wounds. When the redness is spreading or even the wound is discharging, or else patient feel unwell or feverish, the gynecologist who has performed the surgery should be consulted.
The patient will get the wounds wet the day after the operation, but she should avoid spas/baths/swimming pools before the sutures are out.
This is usually because of the colpotomy which was done during the procedure and could last about few days. Upto four week after surgery patient should avoid sex, tampons and strenuous exercise whilst she continue to be bleeding. It is not uncommon that some women notice the stitch material (Vycril or PDS etc.) which is used to close the the vaginal opening inside the abdomen may fall out after a couple of weeks. It might look like a black bit of thread or fishing line. Patient should not be afraid after seeing this thread that what and why should this happen. Although she should not pull on any thread that seems attached inside the vagina.
This can be because of the anesthetic or analgesics agent used especially ones for example Panadeine or morphin. Patient should avoid operating machinery, making important decisions or driving a vehicle for at least 48hrs after surgery. Patient need to take a minimum of two weeks off work, or longer if her work involves the strenuous physical activity or using machinery during her day to day work. The patient should also avoid strenuous exercise for around few weeks.
The patient will need to consult gynecologist again after seven days to achieve the stitches removed. Patient will be offered a scheduled appointment at the hospital in again around 6 weeks.