

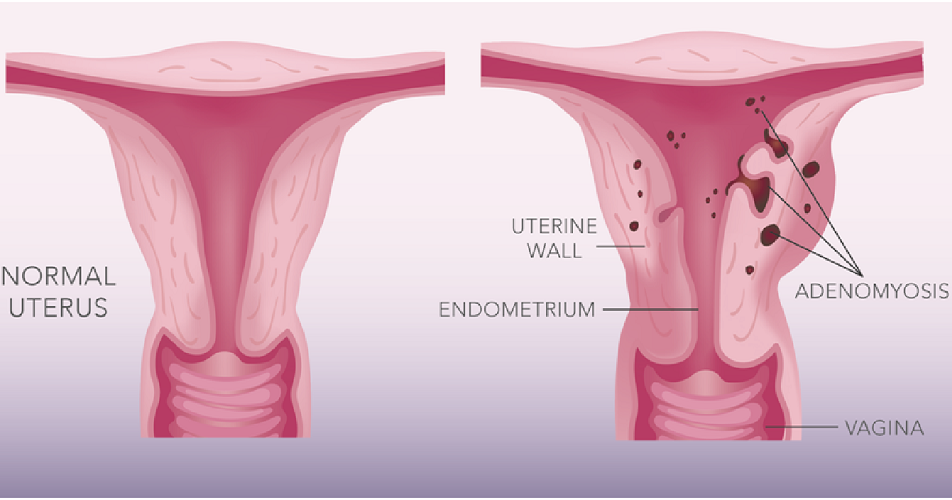
Adenomyosis (ad-uh-no-my-O-sis) occurs when endometrial tissue, which normally lines the uterus, exists within and grows into the muscular wall of the uterus. The displaced endometrial tissue continues to act as it normally would — thickening, breaking down and bleeding — during each menstrual cycle. An enlarged uterus and painful, heavy periods can result.
Symptoms most often start late in the childbearing years after having children.
The cause of adenomyosis remains unknown, but the disease typically disappears after menopause. For women who experience severe discomfort from adenomyosis, certain treatments can help, but hysterectomy is the only cure.
Sometimes, adenomyosis is silent — causing no signs or symptoms — or only mildly uncomfortable. In other cases, adenomyosis may cause:
Your uterus may get bigger. Although you might not know if your uterus is enlarged, you may notice that your lower abdomen seems bigger or feels tender.
The cause of adenomyosis isn't known. Expert theories about a possible cause include:
Regardless of how adenomyosis develops, its growth depends on the circulating estrogen in a woman's body. When estrogen production decreases at menopause, adenomyosis eventually goes away.
Adenomyosis is found in the muscle wall of the uterus. It occurs when the inside lining of the uterus (endometrium) shows within the muscular wall of the uterus. Women may describe heavy and painful periods, and a specialist may notice a ‘bulky’ or ‘boggy’ uterus on examination. Unless severe, adenomyosis may be difficult to accurately diagnose. Vaginal ultrasound scan and MRI have become increasingly useful, and diagnosis is usually made using a combination of a patients history, examination findings and pelvic imaging. Treatment for adenomyosis is complex, and a review with a specialist in this area is recommended. A hysterectomy (removal of the uterus) may be recommended if a women’s family is complete and other strategies have been unsuccessful.
Adhesions are bands of fibrous scar tissue (sometimes they look like rubber bands and or cobwebs) which cause internal organs or tissue to stick together. For example, the ovary to the pelvic side wall. They most commonly present as a result of inflammation or surgery. Some adhesions are congenital (present from birth). They are often seen with endometriosis. Adhesions are normally removed during surgery and precautions taken to prevent development.
Paracetamol belongs to a group of medicines called simple analgesics and helps alleviate mild-moderate pain. Taking an anti-inflammatory either in combination or instead of is sometimes recommended. Codeine is a stronger pain reliever and blocks pain signals from nerves in your body. It can be used alone or in combination with Paracetamol and anti-inflammatories. ALWAYS seek professional advice.
These are anti-inflammatory medications which can help relieve the cramping type of pain associated with periods resulting in less pain, swelling, and inflammation. Anti-inflammatories work better if taken about 24 hours before you expect the pain to occur, otherwise the medication cannot block the pain-producing chemicals as they have already been released. Take anti-inflammatory medications with food as they can cause stomach/gastric irritation. Taking an anti-inflammatory medication and other pain relief can be effective but requires expert advice from your health professional.
The contraceptive pill is often used as a first line treatment to regulate periods and reduce symptoms. There are many different types of ‘pills’ and some are much better suited to help with period pain and endometriosis. Taking the pill continuously decreases the number of periods per year however it can also mask symptoms and the progression of endometriosis. For this reason, recent thoughts are that prescribing pills ‘back to back’ may not be wise if there is no diagnosis. The pill is not suitable for everyone for many reasons (age, cultural, health, choice etc).
An IUD (intrauterine device) e.g. Mirena® is a tiny T-shaped device that releases progesterone (levonogestrel) directly to the uterus. The progesterone acts locally in the uterus and only a small amount is transferred to the bloodstream. The Mirena® IUD provides contraception for up to 5 years and generally stops periods or makes them lighter and has the added benefit that it can also reduce pain and halt the progression of endometriosis.
GnRH (Gonadotrophin Releasing Hormone) analogues are a range of medicines that, when used continuously for longer than 2 weeks cause very little oestrogen to be produced. This deprives the endometrional implants of oestrogen causing them to degenerate. They are usually given as a long-acting injection once a month for up to 6 months. While on GnRH analogues your periods usually stop, therefore can help reduce painful periods. Unpleasant side effects can be experienced..